Electroanalgesia in Contemporary Pain Management: A Comprehensive Exploration
Introduction: Pain management in the contemporary medical landscape has undergone a paradigm shift with the advent of electroanalgesia. This article endeavors to provide a comprehensive examination of electroanalgesia, elucidating its theoretical underpinnings, clinical applications, and potential implications for the future of pain therapeutics.
Theoretical Foundations of Electroanalgesia: Electroanalgesia operates on the principle of modulating the transmission of pain signals through precisely administered electrical currents. Rooted in gate control theory and neuromodulation principles, this approach seeks to exert control over the intricate network of nociceptive pathways, offering a sophisticated intervention for pain mitigation.
Neurophysiological Mechanisms: The neurophysiological mechanisms underpinning electroanalgesia involve the activation of Aβ fibers, triggering inhibitory interneurons and subsequently closing the pain gate. Additionally, the stimulation of descending inhibitory pathways contributes to the attenuation of pain perception. This intricate interplay positions electroanalgesia as a scientifically nuanced intervention.
Clinical Applications Across Pain Modalities: Electroanalgesia exhibits remarkable versatility in its clinical applications, spanning various pain modalities. From neuropathic pain syndromes to musculoskeletal disorders, its efficacy has been demonstrated across diverse clinical spectra. Moreover, its integration into multimodal pain management approaches has showcased synergistic benefits, enhancing overall patient outcomes.
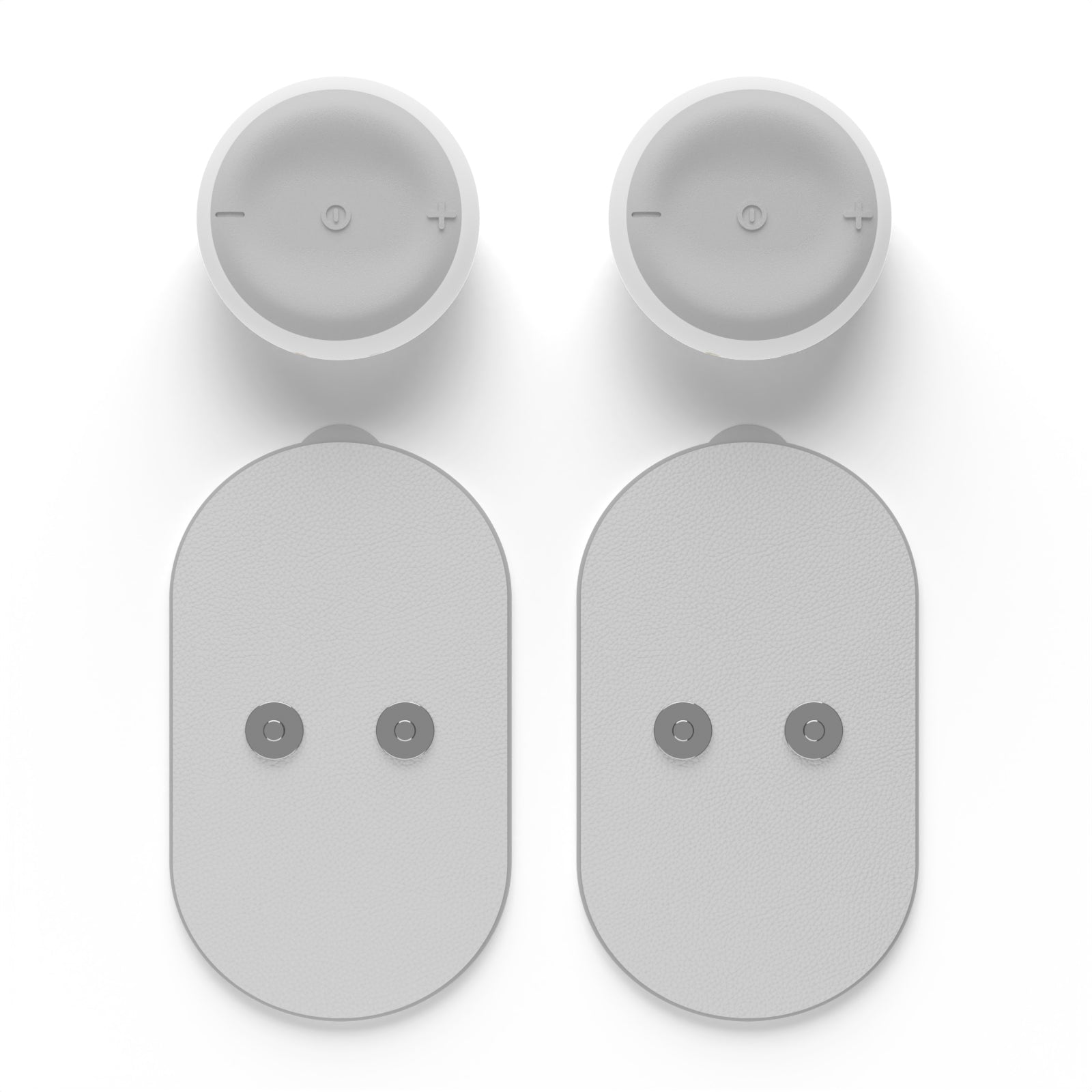
Technological Advancements and Modalities: The evolution of electroanalgesic modalities has been marked by technological advancements, including transcutaneous electrical nerve stimulation (TENS), interferential current (IFC), and pulsed electromagnetic field (PEMF) therapy. These modalities, with their distinct waveform characteristics and targeted applications, underscore the sophistication of contemporary electroanalgesic interventions.
Research Landscape and Evidentiary Support: The scientific community has increasingly focused on substantiating the efficacy of electroanalgesia through rigorous clinical trials and research endeavors. Meta-analyses and systematic reviews have yielded evidence supporting its role in acute and chronic pain management. However, ongoing research seeks to refine protocols, optimize parameters, and ascertain its long-term effectiveness.
Considerations for Clinical Implementation: While electroanalgesia holds substantial promise, its clinical implementation necessitates meticulous considerations. Individual patient profiles, contraindications, and personalized therapeutic regimens must be meticulously evaluated. This ensures not only the maximization of therapeutic benefits but also the mitigation of potential adverse effects.
Future Trajectories: Integration into Precision Pain Medicine: As we stand at the cusp of the fourth industrial revolution in healthcare, electroanalgesia emerges as a potential cornerstone in the trajectory of precision pain medicine. Tailoring interventions based on individual pain phenotypes, genetic predispositions, and real-time physiological feedback heralds a future where electroanalgesia aligns seamlessly with the ethos of personalized medicine.
Conclusion: In conclusion, electroanalgesia epitomizes the convergence of advanced neurophysiological understanding and technological innovation in contemporary pain management. Its nuanced approach, supported by a robust evidence base, positions it as a pivotal modality in the armamentarium of pain therapeutics. The ongoing trajectory of research and clinical integration underscores the transformative potential of electroanalgesia in shaping the future landscape of pain management.